|
A 25 year-old woman presented with headaches. |
![]()
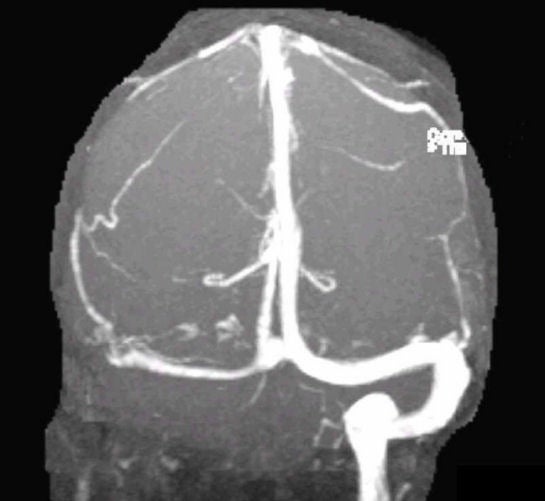
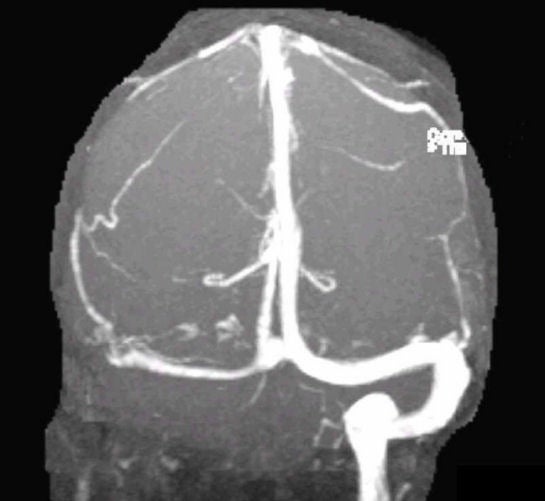
| Cerebral Venous Thrombosis. Magnetic Resonance Venogram
(MRV).
Note the absence of the left sigmoid sinus, as well as the complete
absence of the left internal jugular vein. The left transverse sinus is
attenuated. Cerebral venous thrombosis (CVT) is an uncommon cause of stroke. As venous outflow is impeded, patients develop venous infarctions which are often hemorrhagic. The etiology of CVT is diverse but most often includes the following: ● Genetic hypercoagulable states (e.g., protein S and C
deficiencies, antithrombin III deficiency, Leiden factor V mutation) Patients typically present with a prominent headache. In addition, thrombosis of the superior sagittal sinus classically presents with bilateral leg weakness, as the superior sagittal sinus is midline. Depending on what other sinuses are thrombosed, there can be a multitude of other focal neurological deficits. Seizures are not uncommon. In addition, blockage of venous outflow commonly results in intracranial hypertension. Papilledema may be seen. CVT can mimic the syndrome of idiopathic increased intracranial pressure (so-called pseudotumor cerebri). CVT is an important diagnosis to recognize, as anticoagulation is indicated to prevent further clot formation. The prognosis of CVT varies, from complete recovery, to residual neurological deficits, to death. |
Revised
11/29/06.
Copyrighted 2006. David C Preston